The subject of gluten is super hot with a lot of conflicting opinion and interest. Even among professionals, you may see different recommendations. One MD says grains destroy your brain, while another says whole “intact” grains are a key to long life. Some fitness and wellness gurus advocate avoiding grains as part the Paleo diet and many have signed on to give up their favorite breads. In spite of the paleo-hype, historically, grains have been part of a human diet for more than 10,000 years maybe a hundred thousand or more. For the vast majority of people, grains are a healthy part of eating, providing fiber, B vitamins, and even some protein, and good fats (when whole grain). I love all grains and fortunately can eat them without any problem at all – I’m so devoted that I even grind my own wheat for bread.
However, not everyone can enjoy grains with abandon. Certainly there are those people who have true IgE-mediated allergies to wheat and possibly to other grains. Wheat allergies are not about gluten necessarily, and wheat isn’t the only source of gluten as we know it (which we’ll get to), but I find it helpful to mention the difference between gluten issues and allergies anytime I talk about this subject. Those allergic to wheat make up a very small percentage of the population – probably less than 1%. Those folks should avoid wheat (or their grain allergen) strictly, since food allergies can cause serious and potentially life-threatening reactions. Cross-contact is also a major concern here, since most bread and pasta items are made with wheat and it’s essential to make sure there has been no contamination of wheat-free foods with wheat.
Since the vast majority of people don’t have wheat allergies, let’s talk about gluten. Gluten is a protein found in wheat (including durum, emmer, spelt, farina, farro, KAMUT® khorasan wheat and einkorn), barley, rye and triticale. It is a functional protein in foods and is used for its ability to give structure to baked goods, as a mock meats, in beer (malt), and as a stabilizer. All grains not mentioned previously are naturally gluten-free, but they could become contaminated if they are processed on shared equipment or in shipping or handling anywhere from the field to fork.
Who might benefit from avoiding gluten?
- Celiac Disease (CD) – CD is a rare autoimmune disease that affects up to 1% of the population. It has some genetic component, but there is also likely an environmental component too. There’s a lot that we do not know about CD. However, we do know that lifelong avoidance is necessary to avoid the chronic gut inflammation that damages the villi of the intestines, leading to malnutrition, chronic digestive issues, and predisposes the individual to infertility, bone loss, and a host of other long-term problems. Anyone who suspects that they may have CD should be tested before eliminating gluten from the diet. Testing can start with a simple blood test and be confirmed by biopsy. Lifelong avoidance is needed for those with CD.
- Inflammatory Bowel Disease (IBD) – Crohn’s and ulcerative colitis are two conditions that fall
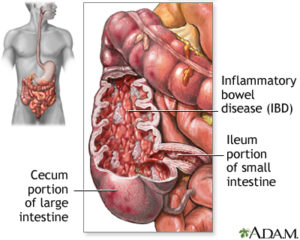
This image shows where and how IBD might manifest, in this case as patchiness in the colon. Source
under the umbrella of IBD. For those with IBD, some research indicates a higher than average prevalence of CD (or vice versa). Those with IBD are already at risk for some of the same long term risks of CD, so those with IBD may benefit from being tested for CD. Trial elimination of gluten, even in the absence of CD may help if other measures fail.
- Non-celiac gluten sensitivity (GS) – GS is another tough to diagnose condition, because there aren’t good tests to identify it. There is even some debate about whether or not it even exists. Primarily diagnosed by an elimination diet, it’s hard to argue with an individual who experiences relief even in the absence of a CD diagnosis. I would advise gluten-elimination in this case only after ruling out all other possible medical conditions to ensure that IBD or CD are not missed. Patients in this category may also actually have IBS and vice versa.
- Irritable Bowel Syndrome (IBS) – IBS is such a tricky condition. Dietary modification can make a big difference, but triggers vary widely by individual (including significant non-food triggers such as stress and smoking). The FODMAP diet may be a helpful way to address potential dietary issues that impact IBD. But the FODMAP diet is not gluten-free. That said, there are some people with IBD who may benefit from avoiding gluten for a while or altogether; these folks may actually belong in one of the categories above and testing should be considered to rule out other disease.
These are the primary groups for which there is good clinical evidence to adopt or consider a gluten free diet. Outside of these groups, I do not generally recommend a gluten-free diet. Why? Because (1) I don’t like to complicate eating unnecessarily; (2) grains are inherently healthy foods; and (3) avoiding gluten may lead to a poorer overall diet with significant nutritional deficiencies, especially among children.
No matter what you may have heard, the evidence is in. Gluten is not the enemy…for most of us anyway.


